Shunt Surgery: A Lifeline for Managing Hydrocephalus
Hydrocephalus, a condition characterized by an excess accumulation of cerebrospinal fluid (CSF) in the brain, can pose significant challenges for those affected. However, thanks to advancements in medical science, shunt surgery has become a crucial lifeline for managing this condition and improving the quality of life for patients.
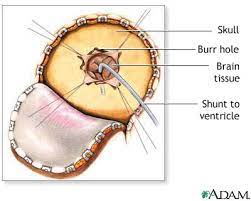
Shunt surgery involves the placement of a thin tube, known as a shunt, into the brain to divert excess CSF away from the affected area. The shunt is connected to another part of the body, typically the abdomen or heart, where the fluid is safely absorbed or drained.
The primary goal of shunt surgery is to restore normal CSF flow and relieve pressure on the brain. By doing so, it helps alleviate symptoms such as headaches, nausea, vision problems, and cognitive difficulties that are often associated with hydrocephalus.
The procedure itself requires meticulous precision and expertise from a skilled neurosurgeon. During surgery, an incision is made in the scalp to access the brain. The surgeon carefully places the shunt system while ensuring it remains secure and functional. Once implanted, regular monitoring and adjustments may be necessary to optimize its performance.
Shunt surgery has revolutionized hydrocephalus treatment by providing long-term management options for patients across all age groups. Infants born with congenital hydrocephalus can undergo this procedure early in life to prevent developmental delays and potential brain damage. Similarly, adults who develop hydrocephalus due to injury or illness can find relief through shunt surgery.
One of the key advantages of shunt surgery is its ability to adapt to individual patient needs. Different types of shunts are available depending on factors such as age, medical history, and specific requirements. Adjustable valves allow healthcare professionals to fine-tune CSF drainage rates based on each patient’s unique needs.
While shunts have greatly improved the lives of many hydrocephalus patients, it’s important to note that they are not without potential complications. Shunt malfunction or blockage can occur, leading to symptoms such as headaches, vomiting, and changes in mental status. Regular follow-up appointments with healthcare professionals are crucial to monitor shunt function and address any issues promptly.
In recent years, advancements in technology have led to the development of programmable shunts that can be adjusted externally using a magnetic device. This innovation offers greater flexibility in managing CSF flow and reduces the need for additional surgeries.
Shunt surgery has undoubtedly transformed the landscape of hydrocephalus treatment. It provides hope and relief to countless individuals living with this condition, allowing them to lead fulfilling lives despite its challenges. Ongoing research and advancements continue to refine surgical techniques and improve outcomes for patients.
If you or a loved one is affected by hydrocephalus, consulting with a specialist is essential. They can assess your unique situation and determine if shunt surgery is a suitable option for managing your condition. With proper care and support, individuals with hydrocephalus can navigate their journey with confidence, knowing that shunt surgery offers a lifeline towards a better quality of life.
Frequently Asked Questions about Shunt Surgery: A Guide to Recovery Time, Purpose, and Living with a Shunt in the Brain
- What is the recovery time for shunt surgery?
- What is a shunt in surgery?
- Can I live a normal life with a shunt?
- Why is a shunt placed in the brain?
What is the recovery time for shunt surgery?
The recovery time for shunt surgery can vary depending on several factors, including the individual patient, the specific type of shunt procedure performed, and any complications that may arise post-surgery. Generally, it is important to remember that recovery is a gradual process and may differ from person to person.
In the immediate aftermath of surgery, patients are typically monitored closely in a hospital setting for a few days. This allows healthcare professionals to assess the initial response to the procedure and ensure proper functioning of the shunt system. During this time, pain medication may be administered to manage any discomfort.
Once discharged from the hospital, patients will continue their recovery at home. It is essential to follow post-operative care instructions provided by the medical team. These instructions may include:
- Incision care: Keeping the surgical site clean and dry while following any specific wound care guidelines provided by healthcare professionals.
- Activity restrictions: Limiting physical activities and avoiding strenuous exercises or heavy lifting as advised by the surgeon.
- Medication management: Taking prescribed medications as directed, including antibiotics or pain relievers if necessary.
- Follow-up appointments: Attending scheduled follow-up visits with healthcare providers for routine check-ups and monitoring of shunt function.
The initial recovery period after shunt surgery typically lasts several weeks to months, during which patients gradually regain their strength and adjust to living with the shunt system. It is important to note that some individuals may experience temporary side effects such as headaches, fatigue, or mild discomfort during this time.
Long-term recovery involves ongoing monitoring of shunt function through regular follow-up appointments with healthcare professionals. These appointments allow for adjustments or revisions if needed and ensure that any potential complications are addressed promptly.
It’s crucial for patients and their caregivers to communicate openly with their medical team throughout the recovery process. Any concerns or changes in symptoms should be reported promptly so that appropriate action can be taken.
Remember that every individual’s recovery journey is unique, and it is important to consult with your healthcare provider for personalized guidance regarding the expected recovery time for your specific case.
What is a shunt in surgery?
In the context of surgery, a shunt refers to a medical device that is used to redirect the flow of bodily fluids from one area of the body to another. Shunts are commonly employed in various surgical procedures to treat or manage specific conditions.
One of the most well-known applications of shunts is in neurosurgery for managing conditions like hydrocephalus, which involves an accumulation of cerebrospinal fluid (CSF) in the brain. In these cases, a shunt system is implanted to divert excess CSF from the brain to another part of the body where it can be absorbed or drained safely.
A typical shunt system consists of several components. It includes a thin flexible tube, known as a catheter, which is inserted into the affected area. This catheter is connected to a valve mechanism that regulates fluid flow and pressure within the shunt system. The other end of the shunt may be placed in a different body cavity, such as the abdomen or heart, depending on the specific procedure and condition being treated.
The purpose of using a shunt in surgery varies depending on the situation. For instance, in cases of hydrocephalus, a shunt helps relieve pressure on the brain by redirecting excess CSF away from it. In other procedures, such as in vascular surgery or dialysis access creation, shunts may be used to establish alternative pathways for blood flow or fluid drainage.
Shunts can be made from various materials, including silicone or other biocompatible substances that minimize adverse reactions within the body. They are designed to remain in place for an extended period and require regular monitoring by healthcare professionals to ensure proper function and address any potential complications.
It’s important to note that while shunts have proven effective in many surgical applications, they do carry some risks. Complications such as infection, blockage, malfunctions, or dislodgement can occur over time and may require further intervention or revision surgery. Regular follow-up appointments with healthcare providers are crucial to monitor the shunt’s performance and address any issues promptly.
Overall, shunts play a vital role in surgical procedures by redirecting bodily fluids and helping to manage specific conditions. They have significantly contributed to improving patient outcomes and quality of life in various medical specialties. The type of shunt used and its specific application depend on the surgical procedure being performed and the unique needs of each patient.
Can I live a normal life with a shunt?
Living a normal life with a shunt is indeed possible for many individuals. Shunt surgery is designed to alleviate the symptoms and complications associated with hydrocephalus, allowing patients to lead fulfilling lives.
With proper management and regular follow-up care, individuals with shunts can engage in various activities, pursue their interests, and maintain a good quality of life. Here are some key points to consider:
- Education and Employment: Many individuals with shunts are able to pursue their education and career goals. It is important to communicate with educational institutions or employers about any necessary accommodations or support that may be required.
- Physical Activities: While certain physical activities may need to be approached with caution, many individuals with shunts are able to participate in sports and exercise routines. It is advisable to consult with your healthcare provider regarding any specific limitations or precautions.
- Social Life: Having a shunt should not hinder your ability to maintain an active social life. Engaging in social activities, hobbies, and spending time with friends and family can all be part of your normal routine.
- Travel: With proper planning and preparation, individuals with shunts can enjoy travel experiences like anyone else. It is recommended to carry important medical information, including details about the shunt, in case of emergencies.
- Regular Check-ups: Ongoing monitoring of the shunt’s function through regular check-ups is vital. Your healthcare provider will assess its performance, make necessary adjustments if required, and address any concerns you may have.
While living a normal life with a shunt is possible for many individuals, it’s important to note that everyone’s experience may vary based on individual circumstances and the underlying condition being treated. Some individuals may require additional precautions or accommodations depending on their specific needs.
It’s crucial to maintain open communication with your healthcare team regarding any changes in symptoms or concerns you may have related to the shunt. By following their guidance and staying proactive in your self-care, you can optimize your chances of leading a fulfilling and normal life with a shunt.
Why is a shunt placed in the brain?
A shunt is placed in the brain to address a medical condition called hydrocephalus. Hydrocephalus occurs when there is an abnormal accumulation of cerebrospinal fluid (CSF) within the brain, leading to increased pressure and potential damage to brain tissue.
The shunt serves as a drainage system, redirecting excess CSF away from the affected area of the brain to another part of the body where it can be safely absorbed or drained. This helps to restore normal CSF flow, relieve pressure on the brain, and prevent further complications associated with hydrocephalus.
By implanting a shunt into the brain, neurosurgeons create a pathway for the excess CSF to be diverted. The shunt typically consists of a thin tube that is inserted into one of the ventricles of the brain (fluid-filled spaces) and then threaded under the skin to another location in the body, such as the abdomen or heart. This allows for continuous drainage and regulation of CSF levels.
The placement of a shunt requires surgical intervention by a skilled neurosurgeon. During the procedure, careful consideration is given to selecting an appropriate location for insertion and ensuring that it remains securely in place. Regular monitoring and adjustments may be necessary after surgery to optimize its performance and address any potential complications.
Overall, placing a shunt in the brain provides an effective means of managing hydrocephalus by alleviating symptoms associated with increased intracranial pressure and promoting normal CSF circulation. It has become a vital treatment option for individuals affected by this condition across different age groups, enabling them to lead healthier lives with improved neurological outcomes.

I like this weblog it’s a master piece! Glad I
noticed this ohttps://69v.topn google.Blog range
Thank you for your positive feedback on our blog article about shunt surgery. We’re glad to hear that you found it valuable. If you have any questions or need more information on the topic, feel free to reach out.